Respiratory Complications in Parkinson’s Disease
Understanding Respiratory Issues
Parkinson’s disease (PD) is primarily known for its impact on motor functions, but it also poses significant non-motor challenges, including respiratory complications. These issues can profoundly affect the quality of life and overall prognosis of individuals with PD. This comprehensive post delves into the various respiratory complications associated with Parkinson’s disease and their management.
Types of Respiratory Complications
1. Obstructive Sleep Apnea (OSA)
OSA is characterized by repeated episodes of partial or complete obstruction of the airway during sleep, leading to disrupted sleep and decreased oxygen levels. PD patients have a higher prevalence of OSA, which manifests as loud snoring, gasping during sleep, excessive daytime sleepiness, and morning headaches. Management includes Continuous Positive Airway Pressure (CPAP) therapy, weight management, positional therapy, and sometimes surgical interventions.
2. Central Sleep Apnea (CSA)
CSA involves pauses in breathing due to the brain’s failure to signal the muscles to breathe. It’s less common than OSA but can occur in PD patients, with symptoms similar to OSA. Treatment involves Adaptive Servo-Ventilation (ASV), addressing underlying heart conditions, and pharmacological treatments.
3. Respiratory Muscle Weakness
PD can weaken the muscles involved in breathing, including the diaphragm and intercostal muscles, leading to shortness of breath, difficulty coughing, increased risk of infections, and hypoventilation. Management includes respiratory muscle training, incentive spirometry, and non-invasive ventilation techniques.
4. Aspiration Pneumonia
Aspiration pneumonia occurs when food, liquid, or saliva is inhaled into the lungs, leading to infection. This is a significant cause of morbidity and mortality in advanced PD due to dysphagia. Symptoms include coughing during or after eating, recurrent infections, and fever. Management involves swallowing therapy, dietary modifications, upright positioning during meals, and in severe cases, gastrostomy feeding tubes.
5. Bronchospasm and Upper Airway Obstruction
These conditions involve the tightening of muscles around the airways and obstruction of the upper airway, often exacerbated by PD medications. Symptoms include wheezing, chest tightness, and shortness of breath. Management includes bronchodilators, adjusting PD medications, and respiratory therapy.
Clinical Management and Therapeutic Strategies
Regular Monitoring
Pulmonary function tests, polysomnography (sleep studies), and regular assessments by pulmonologists and neurologists are essential.
Pharmacological Interventions
Adjusting dopaminergic medications to optimize motor function without exacerbating respiratory symptoms and using medications to manage comorbid conditions like heart failure or COPD.
Rehabilitation and Therapy
Respiratory therapy, exercises to strengthen respiratory muscles, and speech and swallowing therapy to prevent aspiration.
Lifestyle Modifications
Encouraging physical activity to maintain muscle strength, smoking cessation, and avoiding respiratory irritants.
Technological Support
Use of CPAP, BiPAP (Bilevel Positive Airway Pressure), or other ventilatory support systems as needed.
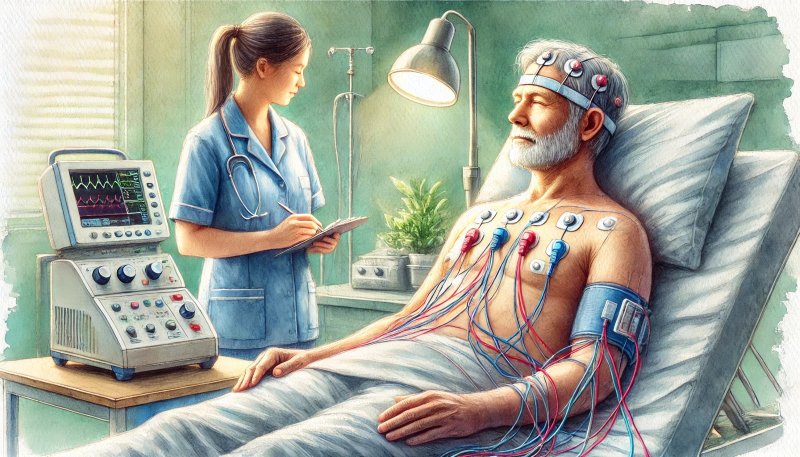
Polysomnogram (PSG)
A polysomnogram is a comprehensive sleep study used to diagnose sleep disorders. It records multiple physiological parameters during sleep, such as brain activity, eye movements, muscle activity, heart rate, respiratory effort, and oxygen levels. For PD patients, a PSG is crucial in identifying sleep apnea, REM sleep behavior disorder, and other sleep-related breathing issues, aiding in tailoring appropriate treatments.
Restrictive Lung Disease
Restrictive lung disease is characterized by reduced lung volume due to stiffness of the lungs or chest wall, muscle weakness, or poor posture, all exacerbated by PD. Symptoms include shortness of breath and fatigue. Diagnosis is made via pulmonary function tests showing reduced lung capacity. Management includes respiratory muscle training, physical therapy to improve posture, and possibly corticosteroids or supplemental oxygen.
Respiratory Dyskinesia
Respiratory dyskinesia is an involuntary and erratic breathing pattern, often resulting from long-term use of levodopa and other dopaminergic medications. Symptoms include erratic breathing and chest discomfort. Management involves adjusting PD medications, considering alternative treatments, and using supportive therapies like respiratory therapy and relaxation techniques.
Conclusion
Managing respiratory complications in Parkinson’s disease requires a multidisciplinary approach, combining regular monitoring, therapeutic interventions, lifestyle modifications, and technological support to improve respiratory health and overall quality of life for individuals with PD.
Keywords
Parkinson’s disease, respiratory complications, obstructive sleep apnea, central sleep apnea, respiratory muscle weakness, aspiration pneumonia, bronchospasm, upper airway obstruction, polysomnogram, restrictive lung disease, respiratory dyskinesia, CPAP therapy, pulmonary function tests, sleep study, respiratory therapy, dysphagia, motor function, non-invasive ventilation, physical therapy.
AI-generated medical content is not a substitute for professional medical advice or diagnosis; I hope you found this blog post informative and interesting. www.parkiesunite.com by Parkie
DALL-E Prompt
A detailed watercolor painting of a person with Parkinson’s disease undergoing a polysomnogram sleep study, surrounded by medical equipment and a caring healthcare professional, capturing the serene and clinical atmosphere.
SEO Keywords: Parkinson’s disease, respiratory complications, sleep apnea, respiratory therapy, polysomnogram