Neuropalliative Care: Comprehensive Support for Neurological Diseases
Neuropalliative care is a specialized field of medicine that focuses on improving the quality of life for patients and families dealing with serious neurological diseases such as Parkinson’s, Alzheimer’s, ALS, and multiple sclerosis. Unlike traditional medical approaches that concentrate solely on treating the disease, neuropalliative care is holistic, addressing not only the medical needs but also the emotional, social, and spiritual aspects of care. This comprehensive approach ensures that patients and their families receive continuous support throughout the entire course of the disease, from diagnosis to advanced stages.
Understanding Neuropalliative Care
Neuropalliative care is designed to alleviate the symptoms and stress associated with neurological diseases, focusing on symptom management, comfort, and overall quality of life. This type of care is crucial for neurological conditions, where symptoms such as pain, mobility issues, cognitive decline, and emotional distress can profoundly impact daily life.
A key feature of neuropalliative care is that it is not limited to end-of-life care. Instead, it is integrated throughout the course of the disease, providing continuous support and adapting to the changing needs and challenges faced by patients and their families as the disease progresses. This ongoing support ensures that patients and families receive the help they need, from the time of diagnosis until the advanced stages of the disease.
Early Integration: From Diagnosis Onward
The integration of neuropalliative care from the moment of diagnosis is vital for several reasons. Early in the disease, this care allows for the prompt identification and management of symptoms, significantly improving the patient’s quality of life. Neurological diseases often present a wide range of symptoms, such as chronic pain, fatigue, mobility issues, and cognitive changes. By addressing these symptoms early, neuropalliative care helps prevent unnecessary suffering and maintains a higher level of functioning for a longer period.
Early integration also fosters a strong therapeutic relationship between the patient, their family, and the care team. This relationship is essential for effective communication, shared decision-making, and the provision of personalized care aligned with the patient’s values, preferences, and goals. From the outset, patients and families are encouraged to discuss their hopes, fears, and expectations, allowing the care team to tailor interventions that support both medical and emotional well-being.
Continuous Support Through the Disease Course
Continuous support through the disease course is administered through a multi-faceted and coordinated approach, involving a range of healthcare professionals, personalized care plans, and ongoing communication with patients and their families. Here’s how this support is typically provided:
1. Interdisciplinary Care Team:
Neuropalliative care is delivered by an interdisciplinary team of healthcare professionals, each bringing specialized expertise to address the complex needs of patients with neurological diseases. The core team typically includes neurologists, palliative care physicians, nurses, social workers, physical and occupational therapists, speech therapists, and spiritual care providers. This team works collaboratively, meeting regularly to review the patient’s condition, adjust care plans, and ensure that all aspects of the patient’s well-being are addressed.
2. Personalized Care Plans:
Each patient receives a personalized care plan that evolves over time as the disease progresses. This plan is tailored to the specific symptoms, preferences, and goals of the patient and their family. It typically includes strategies for controlling pain, fatigue, mobility issues, cognitive decline, and other symptoms. The care plan is revisited and adjusted as needed, ensuring it remains aligned with the patient’s evolving needs and desires.
3. Regular Monitoring and Follow-Up:
Continuous support requires regular monitoring of the patient’s condition and consistent follow-up appointments. This includes routine check-ins, symptom tracking, and crisis intervention when necessary. The care team is available to respond to acute issues or crises, such as sudden changes in symptoms, emotional distress, or the need for emergency care.
4. Patient and Family Education:
Education is a key component of continuous support. Patients and their families are provided with the information they need to understand the disease, manage symptoms, and make informed decisions about care. This includes disease education, symptom management techniques, and caregiver training. Education is delivered in various formats, such as one-on-one sessions with healthcare professionals, printed materials, and online resources.
5. Communication and Coordination:
Effective communication and coordination are vital to the success of continuous support. The care team meets regularly to discuss the patient’s status, review the care plan, and ensure that all team members are aligned in their approach. Open lines of communication between the care team, patients, and families are maintained, allowing for immediate updates on the patient’s condition and ensuring that everyone is on the same page regarding treatment decisions.
6. Access to Support Services:
Patients and families are provided with access to a range of support services, including counseling and support groups, respite care, and financial and legal assistance. These services are designed to reduce the burden on patients and families, ensuring that they have the resources they need to cope with the challenges of the disease.
7. End-of-Life Care:
As the disease progresses to its advanced stages, the focus of neuropalliative care may shift more toward end-of-life care, ensuring that the patient’s final days are as comfortable and peaceful as possible. This includes hospice care coordination and bereavement support for families after the patient’s passing, helping them cope with grief and loss.
Benefits of Neuropalliative Care
The benefits of neuropalliative care are extensive. For patients, it leads to better symptom management, improved emotional well-being, and a higher quality of life. For families, it provides essential support, reducing caregiver burden and helping them navigate the complexities of the disease. Research has shown that patients who receive palliative care often experience better outcomes, including fewer hospitalizations and a greater sense of control over their care. Importantly, neuropalliative care empowers patients and families to make informed decisions about their treatment, aligning care with their values and goals.
Conclusion
Neuropalliative care represents a compassionate and holistic approach to managing serious neurological diseases. By addressing the full range of physical, emotional, and spiritual needs, this specialized field of medicine enhances the quality of life for patients and their families. As awareness and integration of neuropalliative care continue to expand, it has the potential to transform the experience of living with a neurological disease, offering comfort, dignity, and support every step of the way.
SEO Keywords: neuropalliative care, neurological diseases, quality of life, holistic care, palliative care
Disclaimer: AI-generated medical content is not a substitute for professional medical advice or diagnosis; I hope you found this blog post informative and interesting. www.parkiesunite.com by Parkie.
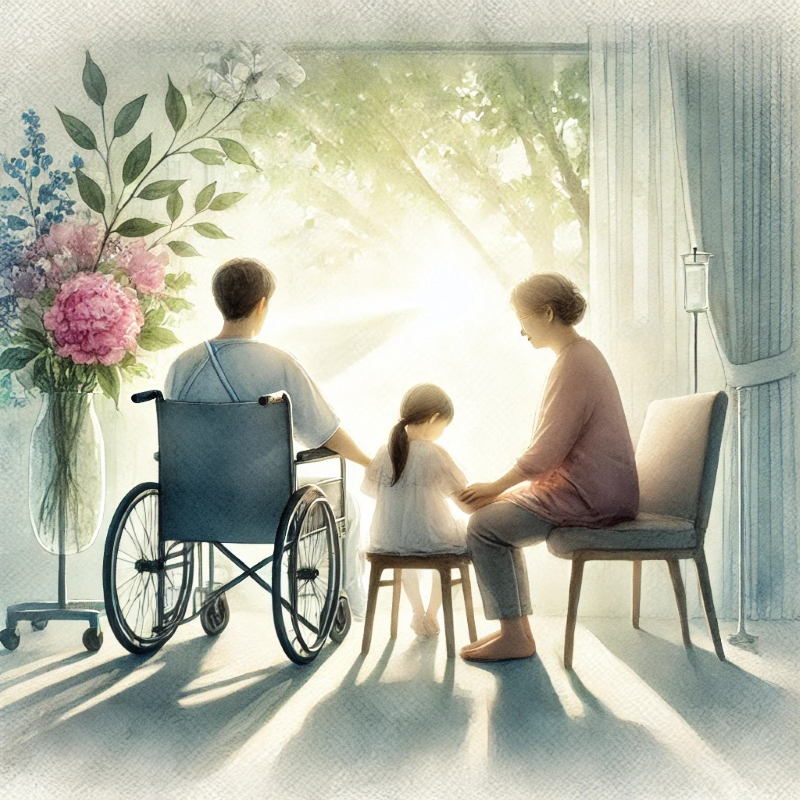
DALL-E Prompt: A serene watercolor painting of a patient and their family sitting together in a sunlit room, with soft light streaming through a window. The scene is peaceful, showing the family in a moment of comfort and connection, with elements of nature, such as flowers or trees, visible through the window.