Understanding Parkinson’s Psychosis
Parkinson’s disease is perhaps best known for its hallmark motor symptoms like tremor and rigidity. However, more than half of individuals with this neurodegenerative disorder will ultimately experience psychosis, a nonmotor symptom that can be particularly unsettling and distressing for both patients and their caregivers.
Psychosis in Parkinson’s can manifest as hallucinations, delusions, or behavioral issues, and significantly impact quality of life and relationships. The ability to communicate openly with healthcare providers about these symptoms is essential for diagnosis and treatment, which may involve adjusting Parkinson’s medications, antipsychotic treatments, or lifestyle changes.
What is Parkinson’s Psychosis?
Psychosis means a loss of contact with reality. Parkinson’s psychosis refers to psychotic symptoms that occur after an established diagnosis of Parkinson’s disease. These symptoms can include:
- Hallucinations: Seeing, hearing, or feeling things that don’t exist, such as people or animals, odors, music, or voices.
- Delusions: Believing something that is not based in reality, like being poisoned by food or medication, or suspecting a trusted person of infidelity or deceit.
Psychosis can also lead to behavioral changes, causing the person to become mean or angry towards loved ones. Hallucinations and delusions can be alarming, and even when patients know these experiences are not real, they can still cause distress.
Causes of Parkinson’s Psychosis
Psychosis in Parkinson’s can arise due to several factors:
- Medication Side Effects: Parkinson’s treatments aim to increase dopamine signaling to manage motor symptoms, but elevated dopamine levels can lead to psychosis.
- Brain Changes: Neurochemical alterations and brain damage due to Parkinson’s itself can contribute to psychosis, especially in cases of Parkinson’s disease dementia.
- Delirium: A state of sudden confusion that affects focus and awareness, often triggered by other medical conditions or changes in medication.
Common Symptoms of Psychosis in Parkinson’s
Psychosis symptoms can vary greatly among individuals with Parkinson’s:
- Hallucinations: Most common in mid- to advanced-stage disease, hallucinations often involve seeing things that aren’t there. Other types include auditory, tactile, olfactory, and gustatory hallucinations.
- Illusions: Brief misperceptions of real objects, like imagining clothes as people.
- Delusions: Irrational or illogical beliefs, such as fears of poisoning or infidelity. These can cause significant distress and lead to unsafe behaviors.
Risk Factors
Risk factors for developing psychosis include:
- Dementia or memory impairments
- Depression or anxiety
- Sleep disorders
- Vision problems
- Advanced age and disease stage
- Medication changes
Importance of Diagnosis and Treatment
Prompt diagnosis and treatment are crucial. Without treatment, psychosis can lead to increased hospitalization risk, care costs, and the need for long-term care. Dr. Michael S. Okun, a medical adviser for the Parkinson’s Foundation, emphasizes the need to recognize and address nonmotor symptoms, such as depression, anxiety, and psychosis, to improve quality of life.
Managing Parkinson’s Psychosis
Treatment of psychosis may involve:
- Medication Adjustments: Balancing motor symptom management with minimizing psychosis.
- Antipsychotic Treatments: These help manage severe psychosis by balancing brain chemicals but must be used cautiously to avoid worsening motor symptoms.
- Therapy and Support: Cognitive behavioral therapy and support groups can help manage symptoms and emotional well-being.
Talking to Your Healthcare Team
Discussing psychosis symptoms with your healthcare team is essential. Up to 90% of people with Parkinson’s may not bring up their psychosis symptoms due to embarrassment or fear. Dr. Rebecca Gilbert, chief mission officer of the American Parkinson Disease Association, encourages patients and caregivers to be proactive in discussing any changes in mood or behavior.
The Impact of Parkinson’s Psychosis on Daily Living
Psychosis can disrupt daily life and relationships, leading to anxiety, depression, and increased fall risks. It can also pose significant challenges for caregivers, who may experience burnout, social isolation, or depression.
Long-term Management
Long-term management may involve regular check-ins with healthcare providers, adherence to medication regimens, and seeking support from family, friends, or support groups. The American Parkinson Disease Association offers resources for managing Parkinson’s psychosis and navigating its challenges.
Conclusion
Parkinson’s psychosis is a complex and often distressing symptom that affects many individuals with the disease. Open communication with healthcare providers and proactive management strategies are essential for improving quality of life and minimizing the impact of psychosis on daily living.
SEO Keywords: Parkinson’s disease psychosis, Parkinson’s symptoms, nonmotor symptoms, hallucinations, delusions
Disclaimer: AI-generated medical content is not a substitute for professional medical advice or diagnosis; I hope you found this blog post informative and interesting. www.parkiesunite.com by Parkie.
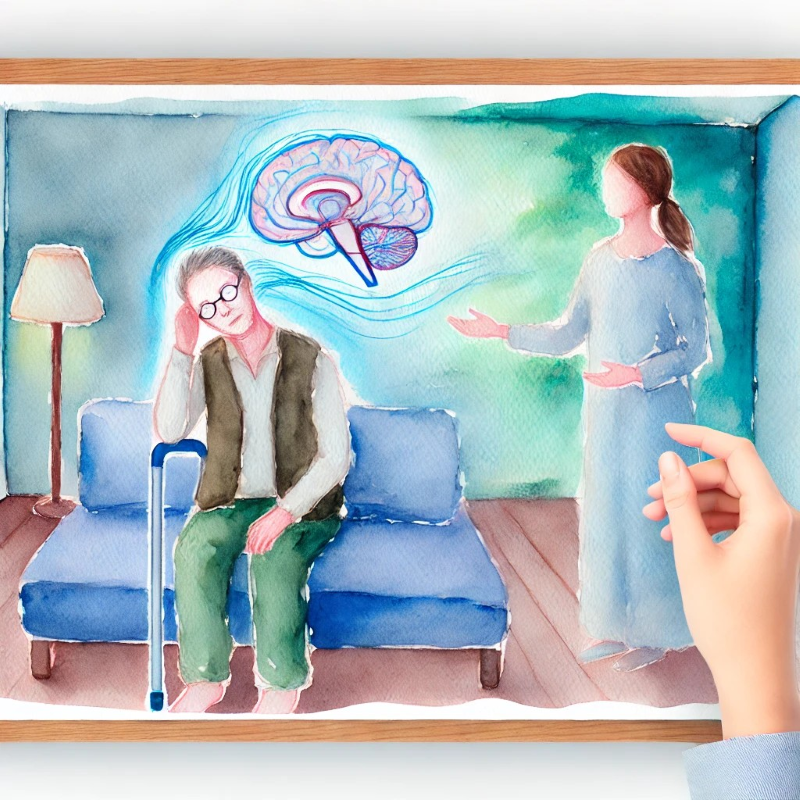
DALL-E Prompt: A watercolor image depicting a serene and gentle portrayal of a person with Parkinson’s disease, showing both motor and nonmotor symptoms like tremor, rigidity, and signs of distress. The setting is a calm and cozy room with soft lighting. A caregiver is nearby, offering support with a warm, compassionate expression. The artwork should reflect empathy, care, and the complexity of living with Parkinson’s psychosis. The colors should be soothing, with shades of blue and green to create a calming atmosphere.