Gut-Brain Axis in Parkinson’s Therapy
Introduction
Research into the gut-brain axis as a therapeutic target for Parkinson’s disease (PD) has grown significantly over the past five years. This literature review provides an overview of current findings linking gut health and neurodegeneration in PD, focusing on gut microbiota’s role, B vitamin deficiencies, and metabolic pathways that contribute to disease progression. Additionally, it highlights gaps in our understanding, particularly regarding age-dependent responses to microbiota-based interventions and the potential for tailored treatments. Studies included in this review were selected using specific search criteria and methodological rigor to ensure a comprehensive synthesis of recent advancements and to outline directions for future research.
Methodology for Source Selection
To compile relevant studies, I conducted a systematic search of electronic databases, including PubMed, ScienceDirect, and JSTOR. The following inclusion criteria were applied: articles published within the last five years, peer-reviewed, focused on PD, gut microbiota, B vitamin metabolism, or the gut-brain axis. Keywords such as “gut-brain axis,” “Parkinson’s disease,” “B vitamins,” “microbiota therapy,” and “neuroinflammation” were used in various combinations to refine the results. Studies meeting these criteria were then evaluated for their contributions to understanding the gut-brain link in PD and were critically assessed to address the review’s objective: examining the role of microbiota in PD management and identifying existing research gaps.
1. Gut-Brain Axis in Neurodegeneration
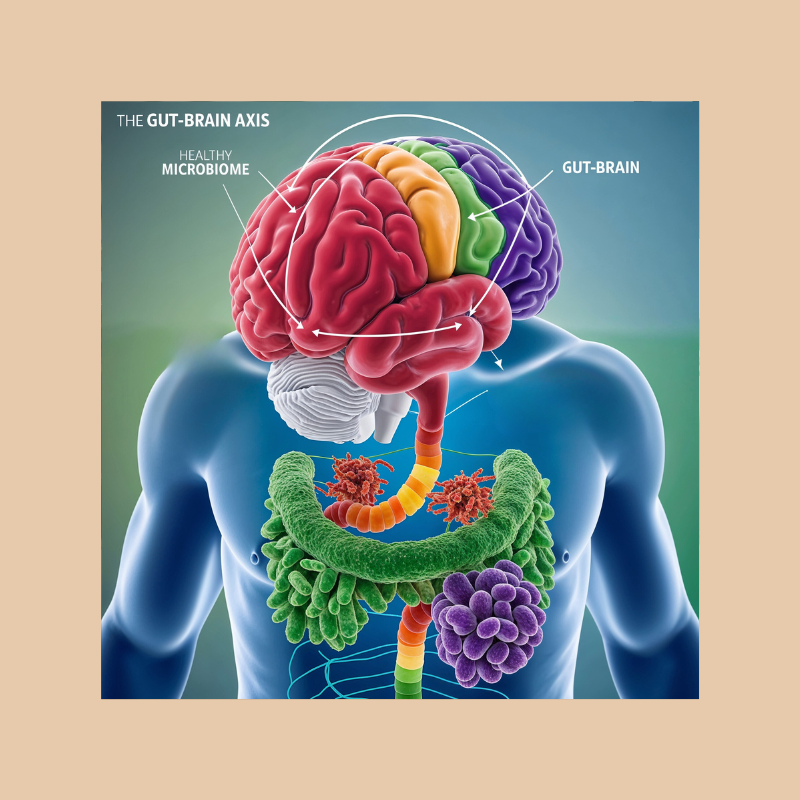
Numerous studies confirm that the gut-brain axis, a bidirectional communication pathway between the gut and central nervous system, plays a critical role in PD progression. This relationship is underscored by findings that gut dysbiosis—a disruption of normal microbiota—can trigger inflammation and oxidative stress, exacerbating PD symptoms. A recent study (Li et al., 2023) demonstrated that gut dysbiosis correlates with increased alpha-synuclein aggregation in PD patients, suggesting that gut health interventions could modulate this aggregation and potentially slow disease progression.
2. Role of Microbiota in B Vitamin Synthesis
Emerging research highlights a deficiency in gut-derived B vitamins, particularly riboflavin (B2) and biotin (B7), as a contributor to PD symptoms. Nagoya University’s study (Nishiwaki et al., 2024) showed a significant reduction in microbial genes responsible for B vitamin synthesis in PD patients. The lack of these vitamins has been linked to reduced levels of short-chain fatty acids (SCFAs) and polyamines, essential for maintaining gut integrity. This connection suggests that supplementing B vitamins may restore gut barrier function and prevent neuroinflammation, thus mitigating PD progression.
3. Short-Chain Fatty Acids and Intestinal Integrity
SCFAs, particularly butyrate, have gained attention for their role in supporting the intestinal barrier. According to Chen et al. (2022), decreased SCFA production in PD patients weakens gut barrier function, increasing intestinal permeability and allowing toxins to enter the bloodstream. This influx of toxins can trigger inflammation in the brain, worsening neurodegenerative symptoms. SCFA supplementation or microbiota interventions that increase SCFA production might therefore offer protective benefits for PD patients.
4. Polyamines and Neuroprotective Mechanisms
Polyamines are small organic compounds with neuroprotective effects, supporting cellular functions and maintaining the blood-brain barrier’s integrity. A study by Wang et al. (2021) found that PD patients exhibited lower polyamine levels, leading to compromised gut and blood-brain barriers. This suggests that enhancing polyamine synthesis in the gut, either through dietary or microbial interventions, may provide an additional avenue for therapy, possibly reducing neurodegeneration in PD.
5. Age-Dependent Responses to Microbiota Interventions
One area that remains underexplored is how age affects the gut’s response to interventions targeting microbiota. Studies suggest that younger PD patients respond more favorably to gut-targeted therapies than older individuals, whose microbiota may have diminished adaptability due to age-related changes. This discrepancy in response rates could be addressed through personalized microbiota-based therapies tailored to the age and metabolic profile of each patient. Further research is needed to determine optimal therapeutic strategies across age groups.
6. Personalized Microbiota Therapy
Personalized therapy based on individual microbiota profiles has gained traction as a promising approach. For instance, Fei et al. (2023) demonstrated that microbiota analysis and targeted supplementation could effectively reduce PD symptoms in a subset of patients with specific gut microbiota deficiencies. Such personalized approaches underscore the importance of identifying each patient’s microbiome profile to optimize treatment outcomes, although more large-scale studies are required to validate this approach.
7. Potential for Probiotic and Prebiotic Interventions
Probiotic and prebiotic therapies offer an additional method to support the gut microbiota, enhancing the gut-brain axis and potentially delaying PD progression. A study by Zhang et al. (2022) demonstrated that specific probiotic strains increased B vitamin production, suggesting that microbiota-enhancing interventions may support gut health. Nonetheless, variability in individual microbiota responses calls for more targeted approaches, particularly among older adults whose microbiota composition is less resilient.
Discussion of Research Gaps
While substantial evidence links the gut-brain axis to PD, several gaps remain:
- Age-Dependent Variability: Few studies address how age-related changes in gut microbiota impact PD progression and the efficacy of microbiota-based therapies. Given the observed differences in response rates, further research is essential to determine how aging alters the gut-brain axis and affects treatment.
- Mechanisms of Microbiota-B Vitamin Interaction: Although B vitamins have shown promise in supporting gut integrity and neuroprotection, the precise mechanisms by which gut bacteria synthesize these vitamins and impact brain health remain unclear. Studies examining these mechanisms could inform better therapeutic strategies.
- Longitudinal Impact of Microbiota Therapy: Many existing studies are short-term, providing limited insights into the long-term efficacy and safety of microbiota-based therapies for PD. Future longitudinal studies could establish the sustainability of these therapies and potential side effects over time.
Conclusion
The gut-brain axis offers a compelling target for Parkinson’s disease management, particularly through microbiota-based interventions that support B vitamin synthesis, SCFA production, and polyamine levels. However, the variability in age-dependent responses, the need for personalized treatments, and the mechanisms linking gut health to neurodegeneration highlight critical areas for further study. Addressing these gaps could refine microbiota-targeted therapies and lead to more effective, individualized approaches to slowing PD progression.
DALL-E Prompt:
“Create a detailed digital image of the gut-brain axis connection with a focus on a healthy human gut microbiome, showing colorful bacterial colonies and a protective barrier around the brain, highlighting pathways between the gut and brain with visual markers. Background includes a soft blue and green gradient to represent health and healing.”
SEO Keywords
Parkinson’s disease, gut-brain axis, microbiota therapy, B vitamins, neuroinflammation
AI-generated medical content is not a substitute for professional medical advice or diagnosis; I hope you found this blog post informative and interesting. www.parkiesunite.com by Parkie