Inflammation and Brain Aging: Gaps and Future Directions
Inflammation plays a critical role in accelerating brain aging and the development of neurodegenerative disorders, including dementia, Parkinson’s disease, and other brain disorders. Despite significant advancements in understanding these inflammatory processes, critical gaps remain, particularly regarding age-dependent responses and their variability across individuals. This literature review synthesizes findings from peer-reviewed research conducted over the past five years, identifies gaps in the current knowledge, and highlights areas for future investigation.
Methodology for Literature Search
To compile this review, databases such as PubMed, Scopus, and Google Scholar were utilized to locate relevant peer-reviewed articles. Search terms included “inflammation and brain aging,” “neurodegenerative diseases and inflammation,” “Parkinson’s disease and chronic inflammation,” and “age-dependent neuroinflammatory responses.” Inclusion criteria were publications from 2018 to 2023 in high-impact journals that addressed the relationship between inflammation and brain disorders. Articles focusing on animal models and human clinical trials were prioritized to ensure a comprehensive understanding.
Current Understanding of Inflammation and Brain Disorders
1. The Role of Neuroinflammation in Brain Aging
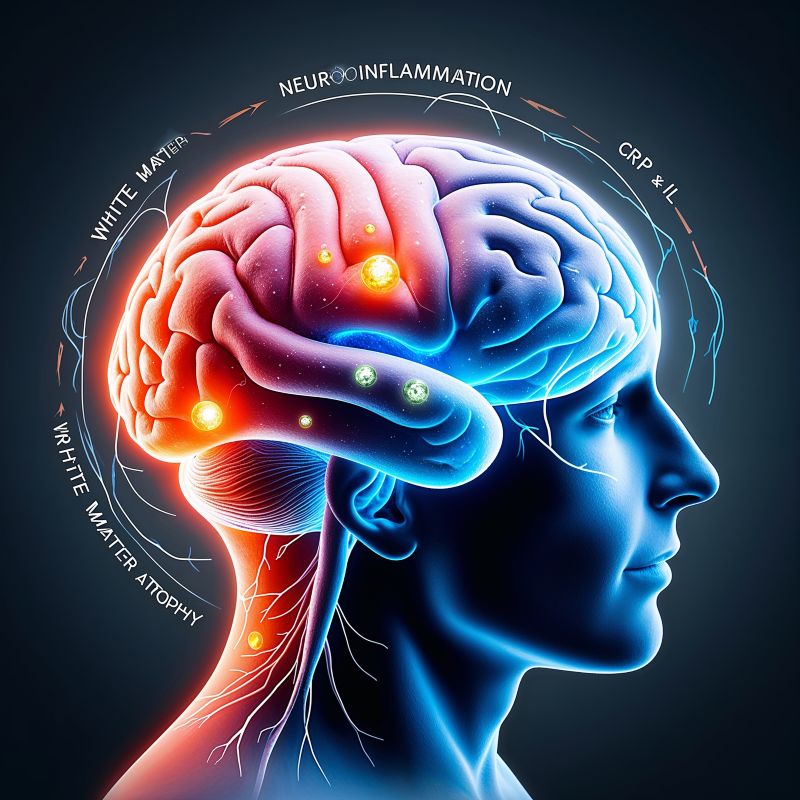
Neuroinflammation, a hallmark of aging, contributes to synaptic loss, white and gray matter atrophy, and cognitive decline. Research shows elevated levels of inflammatory markers such as C-reactive protein (CRP) and interleukin-6 (IL-6) in older adults with mild cognitive impairment (MCI) and dementia. Chronic inflammation exacerbates oxidative stress, mitochondrial dysfunction, and vascular changes, accelerating brain aging (Lavretsky et al., 2020; Stappenbeck et al., 2022).
2. Parkinson’s Disease and Inflammatory Processes
In Parkinson’s disease (PD), neuroinflammation is linked to dopaminergic neuron loss and α-synuclein aggregation. GLP-1 receptor agonists, such as lixisenatide, have shown promise in reducing inflammation and slowing disease progression. However, the exact mechanisms by which inflammation contributes to disease heterogeneity in PD remain unclear (Frankovich et al., 2021; Lixipark Consortium, 2023).
3. Cognitive Decline and Systemic Inflammation
Studies suggest a strong association between systemic inflammation and cognitive decline. Longitudinal data from the Neurology journal revealed that elevated CRP levels in early adulthood correlate with memory deficits in midlife (Xu et al., 2021). Similarly, childhood chronic inflammation has been linked to increased risk of depression and psychosis, underscoring the importance of early intervention (JAMA Psychiatry, 2023).
Gaps in the Current Research
1. Age-Dependent Inflammatory Responses
One of the most pressing gaps is the limited understanding of how age modulates inflammatory processes. Research often assumes uniform responses to inflammation across different age groups, which may not accurately reflect reality. Identifying biomarkers specific to age-related inflammatory changes could pave the way for tailored interventions.
2. Variability in Neuroinflammatory Mechanisms
Significant interindividual variability exists in the progression and impact of neuroinflammation. Genetic predispositions, environmental exposures, and lifestyle factors such as diet and exercise are poorly understood in this context. Future research should explore how these factors interact with age-dependent inflammation.
3. Lack of Longitudinal Human Studies
Most studies on inflammation and brain aging rely on animal models or cross-sectional data. While these methods provide valuable insights, they fail to capture the long-term trajectory of neuroinflammation and its impact on human aging. Large-scale, longitudinal human studies are essential to fill this gap.
4. Intersection of Inflammation and Comorbidities
Inflammation often coexists with comorbidities such as diabetes, cardiovascular disease, and obesity, which also influence brain health. The interplay between these conditions and neuroinflammation warrants deeper exploration to develop holistic treatment strategies.
Future Directions for Research
- Developing Age-Specific Interventions: Future therapies should account for age-related differences in inflammatory responses to optimize outcomes.
- Personalized Medicine Approaches: Incorporating genetic and lifestyle factors into treatment plans can address individual variability in neuroinflammatory pathways.
- Advanced Biomarker Identification: Developing non-invasive biomarkers to monitor chronic inflammation and its impact on the brain is critical for early detection and intervention.
- Integrating Multidisciplinary Research: Combining neuroscience, immunology, and systems biology can provide a more comprehensive understanding of neuroinflammation and its consequences.
Conclusion
While the connection between inflammation and brain disorders like dementia and Parkinson’s disease is well-established, significant gaps remain in understanding age-dependent responses, individual variability, and the interplay with comorbidities. Addressing these gaps through longitudinal studies, personalized medicine, and advanced biomarker development will be pivotal in mitigating the effects of inflammation on brain health.
AI-generated medical content is not a substitute for professional medical advice or diagnosis; I hope you found this blog post informative and interesting. www.parkiesunite.com by Parkie
DALL-E Prompt
“An artistic depiction of neuroinflammation in the human brain, showing glowing inflammatory markers like CRP and IL-6, with highlighted pathways leading to gray and white matter atrophy. The illustration should convey a futuristic, scientific visualization in vibrant blue, orange, and green hues, set against a dark gradient background.”
SEO Keywords
inflammation and brain aging, dementia and inflammation, Parkinson’s neuroinflammation, chronic inflammation and brain health, cognitive decline markers